Global Spine J. 2021 May;11(4):515-524. doi: 10.1177/2192568220914883.Epub 2020 Mar 27.
Alexander Von Glinski, Christopher J Elia, Ariel Takayanagi, Emre Yilmaz, Basem Ishak, Joe Dettori, Benjamin A Schell, Erik Hayman, Clifford Pierre, Jens R Chapman, Rod J Oskouian
Abstract
Study design: Retrospective cohort study.
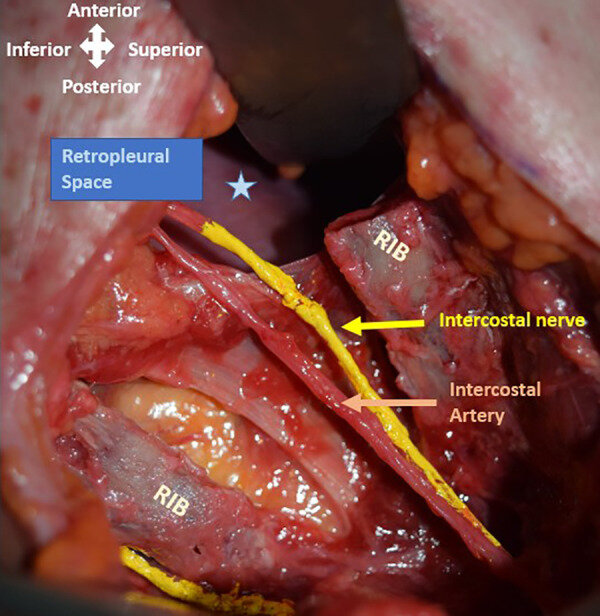
Objective: Complication profiles for lateral approaches to the spine are well established. However, the influence of level of surgery on complication rates and subtypes are less well established. To determine risk factors for complications as determined by level and surgery type in patients undergoing a lateral (retroperitoneal or retropleural approach) to the thoracolumbar spine.
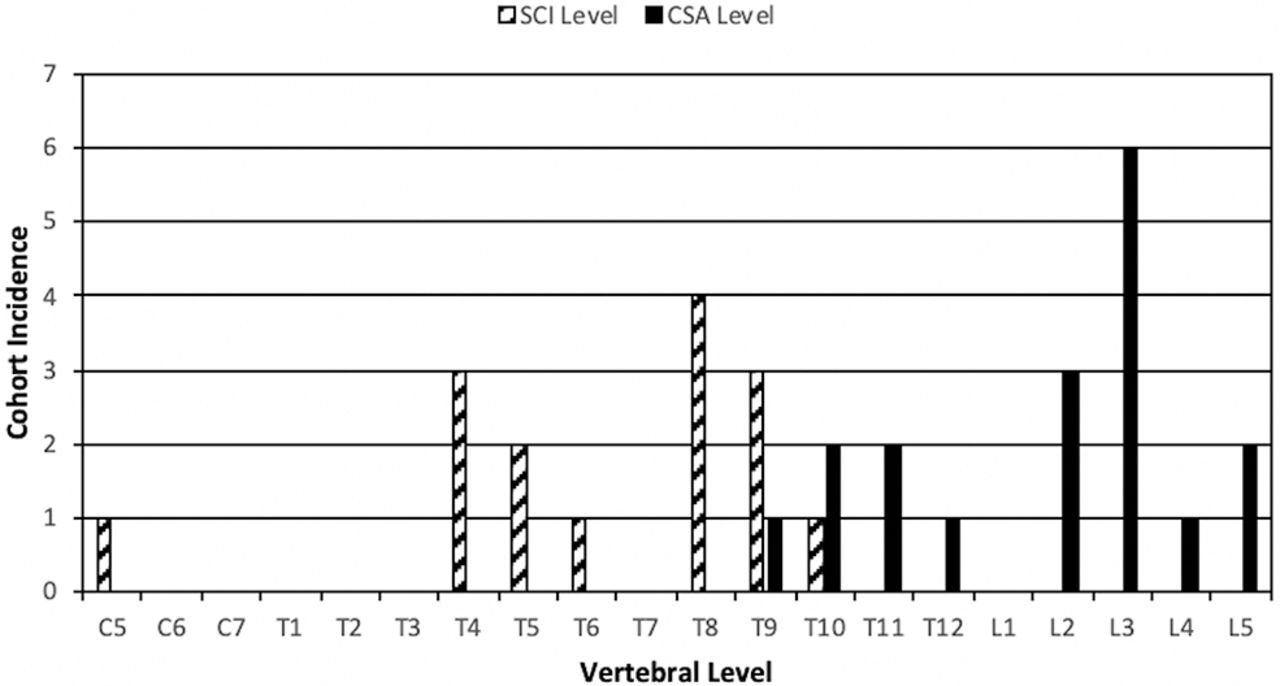
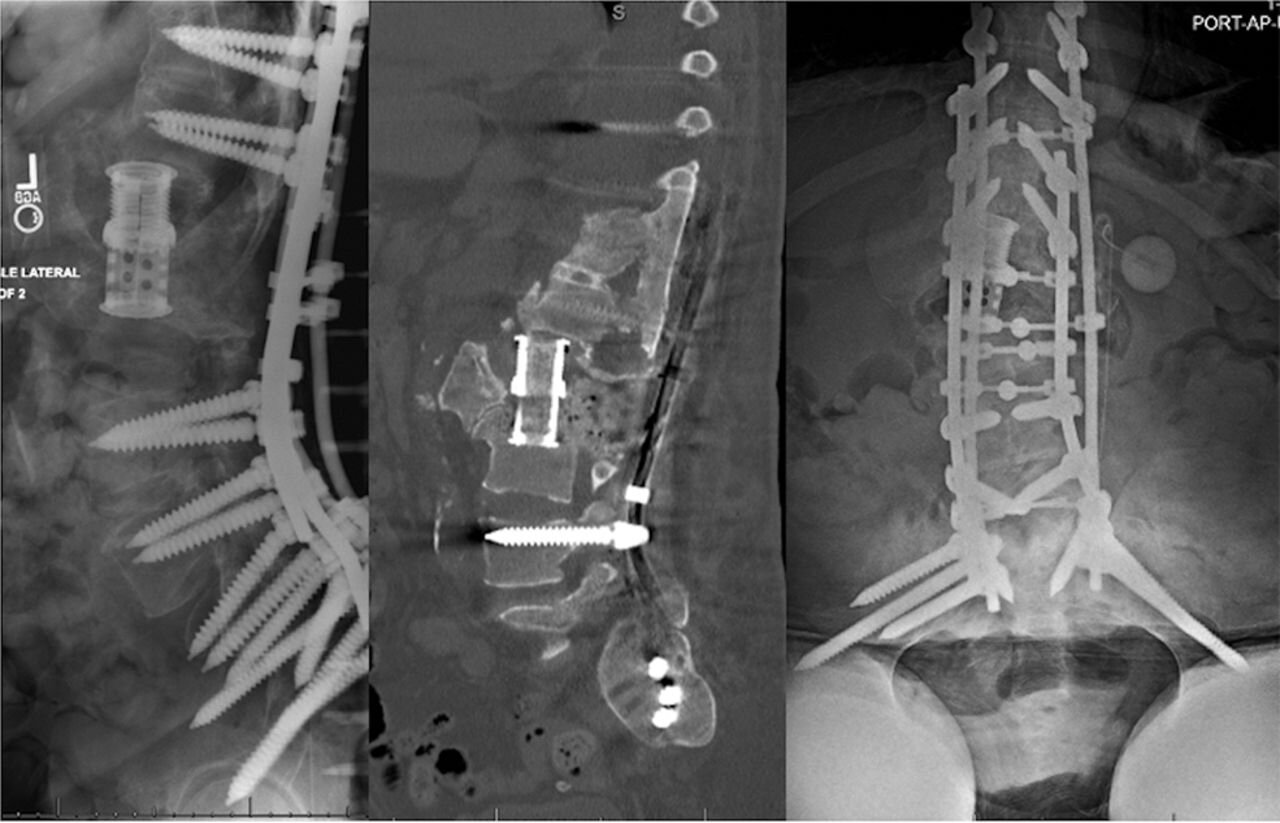
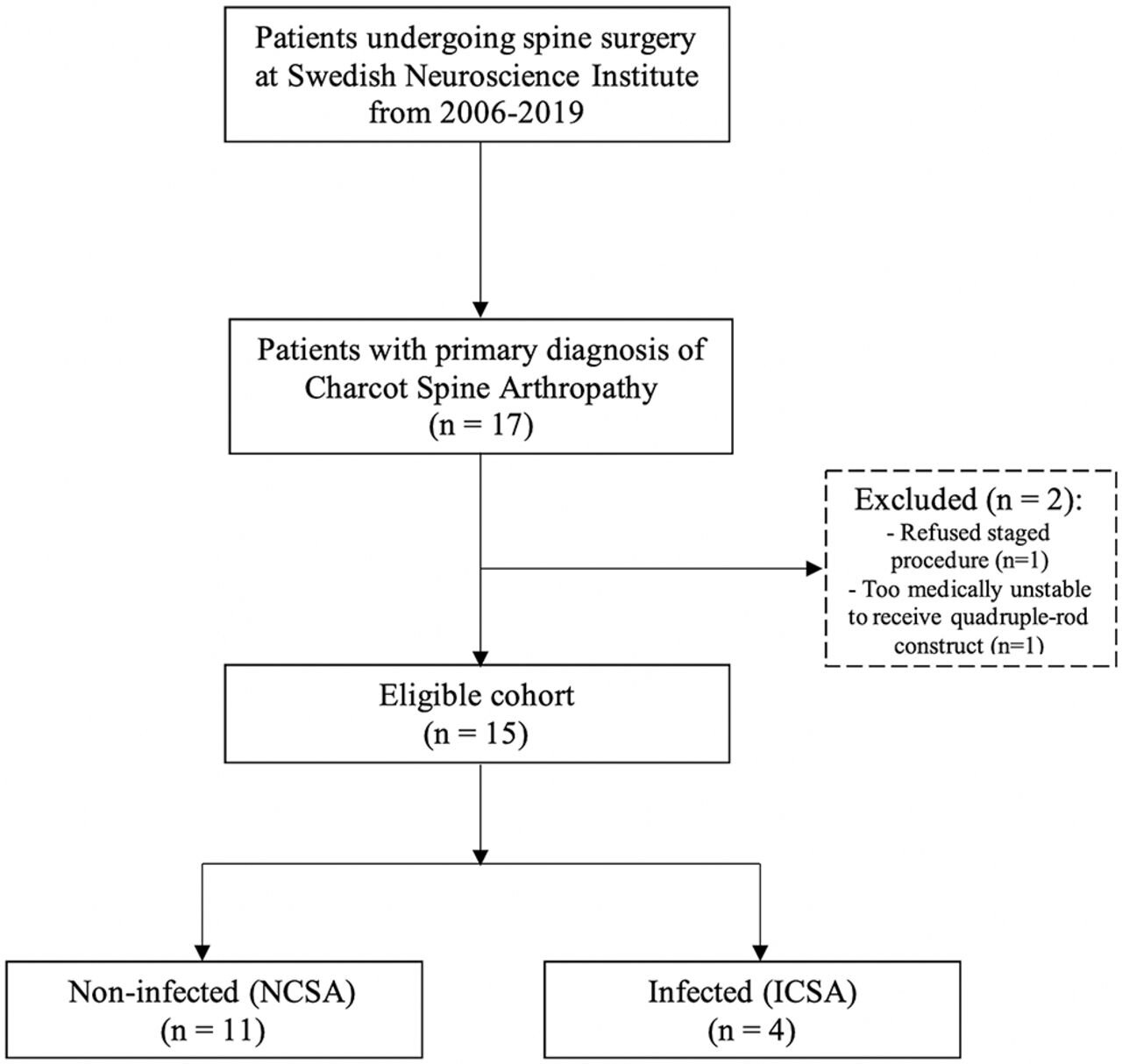
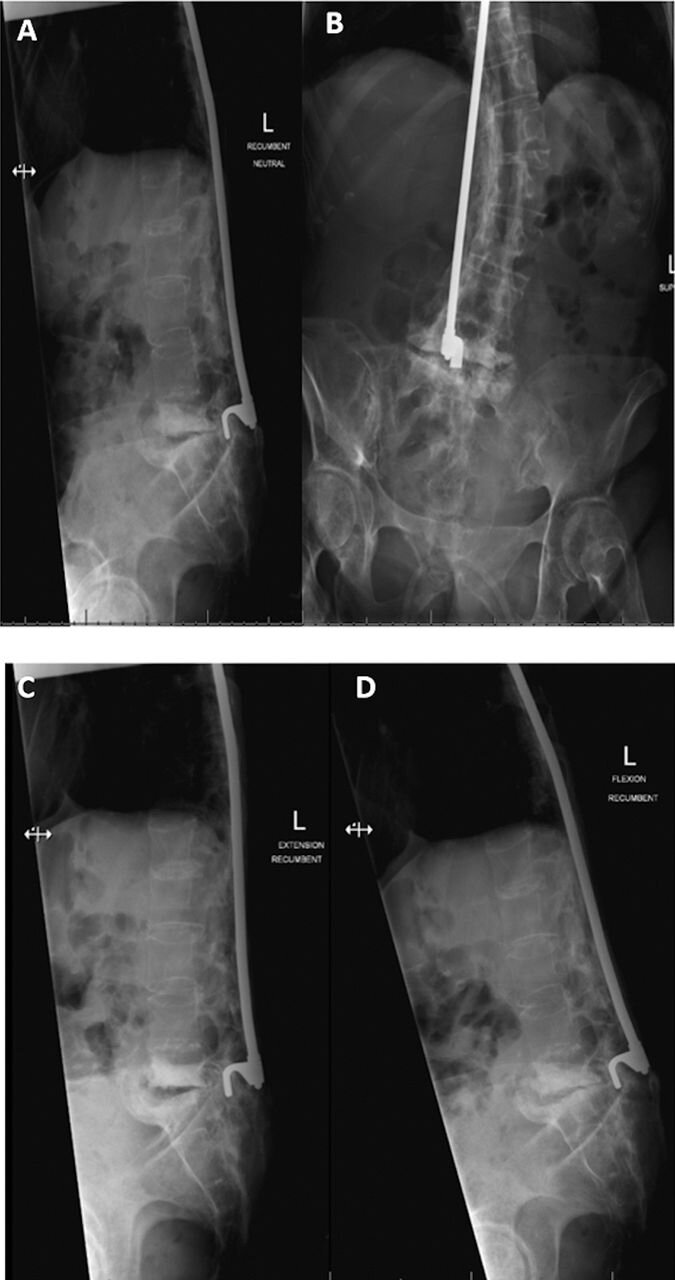
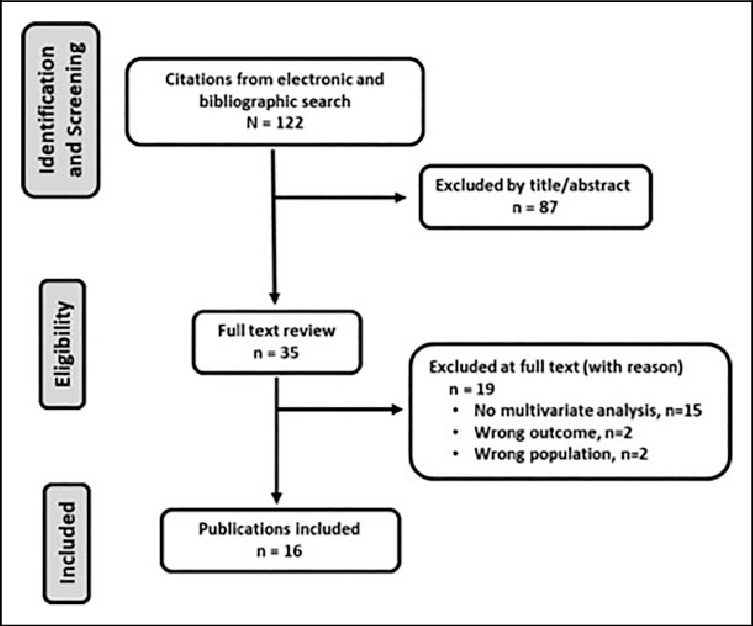
Methods: All adult patients undergoing a lateral thoracolumbar fusion with or without posterior instrumentation performed at a single institution were identified. Primary outcomes assessed were presence of complication, complication subtype, and need for reoperation. The primary independent variables were spinal level (thoracic, thoracolumbar, or lumbar) and type of surgery (discectomy or corpectomy). Categorical outcomes were compared using chi-square test. Unadjusted and adjusted odds ratios for corpectomy status were calculated to determine risk of complication by level. P < .05 was considered statistically significant.
Results: A total of 165 patients aged 18 to 75 years were identified as having undergone a lateral fusion. Complication rates were 28.6%, 36.4%, and 11% for thoracic, thoracolumbar, and lumbar lateral approach fusions, respectively. Under univariate analysis, patients undergoing lateral approach in the thoracic spine group had significantly higher rates of postoperative complications than those in the lumbar group (P = .005). After adjusting for corpectomy status, there was no difference in complication rates.
Conclusions: Lateral (retroperitoneal or retropleural) approaches to the thoracic and thoracolumbar spine may be used with complication rates comparable to well-established lumbar approaches. Extent of surgery (corpectomy vs discectomy) rather than level of surgery may represent the primary driver of complications.
Keywords: complication; corpectomy; discectomy; lateral approach; neurologic deficit; pneumothorax.