Abstract
BACKGROUND:
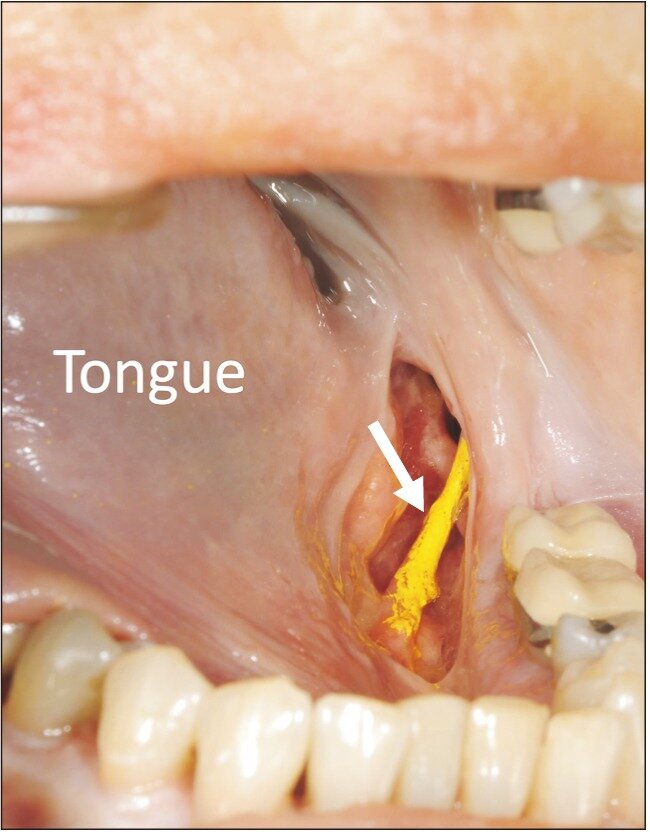
When it comes to autogenous nerve grafting, the sural and great auricular nerve (GAN) are the 2 nerves predominately used for trigeminal and facial nerve repair. Arising from the second and third cervical ventral rami, the GAN emerges from the posterior border of the sternocleidomastoid coursing superiorly and anteriorly toward the ear.
METHODS:
Eleven sides from 5 Caucasian and 1 Asian cadaveric heads (all fresh-frozen) were used. One man and 5 women were used with an age at death ranging from 57 to 91 years, with a mean of 80.3 years. Measurements were made from the inferior border of the ear to the GAN, the GAN to the external jugular vein, and the inferior border of the mastoid process to the GAN; the proximal, medial, and distal diameters of the GAN and the length of the GAN that was obtained from this exposure were also measured.
RESULTS:
The mean distance from the inferior border of the mastoid process to the GAN, inferior border of the ear to the GAN, and GAN to the external jugular vein was 27.71, 31.03, and 13.28 mm, respectively. The mean length of the GAN was 74.86 mm. The mean diameter of its distal, middle, and proximal portions was 1.51, 1.38, and 1.58 mm, respectively.
CONCLUSIONS:
The GAN is an excellent option for use in nerve grafting for repair of, for example, facial dysfunction. In this study, we review our measurements, techniques for identification, and dissecting techniques for the GAN. The proximity to the operative area and minimal complications associated with GAN grafting might contribute to improved patient satisfaction and better outcomes regarding functional restoration.
Copyright © 2019 Elsevier Inc. All rights reserved.
KEYWORDS:
External jugular vein; Great auricular nerve; Nerve graft; Sternocleidomastoid